Understanding Mental Disorders
What Is Psychological Abnormality
While many definitions of abnormality have been proposed over the years ,none has won total acceptance. Still, most of the definitions have certain features in common, often called the “four Ds” : deviance, distress, dysfunction, and danger. That is the pattern of psychological abnormality are typically deviant (different, extreme,unusual, perhaps even bizarre), distressing(unpleasent and upsetting to the person), dysfunctional (interfering with the person’s ability to conduct daily activities in a constructive way), and possibly dangerous. There also duration that needs to be considered.
SCHIZOPHRENIA
Schizophrenia is a chronic mental disorder characterized by significant disruptions in thought, perception, emotion, and behavior. It often includes delusions, hallucinations, disorganized thinking, and negative symptoms.
DSM-5 Criteria (Summarized):
Two or more of the following symptoms must be present for a significant portion of time during a one-month period. At least one must be delusions, hallucinations, or disorganized speech:
1. Delusions
2. Hallucinations
3. Disorganized speech
4. Grossly disorganized or catatonic behavior
5. Negative symptoms
6.Continuous signs of disturbance must persist for at least six months.
7.Impaired functioning in work, relationships, or self-care must be evident.
8.The symptoms must not be due to substance use or another medical condition.


BIPOLAR DISORDER
Bipolar I Disorder is a mood disorder characterized by the occurrence of at least one manic episode, which may be preceded or followed by hypomanic or depressive episodes.
DSM-5 Criteria (Manic Episode):
A distinct period of abnormally elevated, expansive, or irritable mood, and increased goal-directed activity or energy, lasting at least one week and present most of the day, nearly every day.
During the mood disturbance, three (or more) of the following are present (four if mood is only irritable):
1. Inflated self-esteem or grandiosity
2. Decreased need for sleep
3. More talkative than usual or pressured speech
4. Flight of ideas or racing thoughts
5. Distractibility
6. Increase in goal-directed activities or psychomotor agitation
7. Involvement in high-risk activities (e.g., spending sprees, sexual indiscretions)
The mood disturbance is severe enough to cause marked impairment in functioning or to require hospitalization.
MAJOR DEPRESSIVE DISORDER
Major Depressive Disorder is a mood disorder marked by a persistent feeling of sadness, emptiness, or irritability, accompanied by a range of physical and cognitive symptoms. It significantly interferes with daily functioning.
DSM-5 Criteria:
Five (or more) of the following symptoms have been present during the same 2-week period and represent a change from previous functioning. At least one of the symptoms must be (1) depressed mood or (2) loss of interest or pleasure:
1. Depressed mood most of the day, nearly every day
2. Markedly diminished interest or pleasure in all or almost all activities
3. Significant weight loss or gain, or change in appetite
4. Insomnia or hypersomnia
5. Psychomotor agitation or retardation
6. Fatigue or loss of energy
7. Feelings of worthlessness or excessive guilt
8. Diminished ability to think or concentrate, or indecisiveness
9. Recurrent thoughts of death, suicidal ideation, or suicide attempt
Symptoms cause significant distress or impairment in social, occupational, or other important areas of functioning.
The episode is not attributable to the physiological effects of a substance or another medical condition.
There has never been a manic or hypomanic episode.


GENERALIZED ANXIETY DISORDER
GAD involves excessive anxiety and worry about various events or activities, occurring more days than not for at least six months.
DSM-5 Criteria:
The individual finds it difficult to control the worry.
Anxiety and worry are associated with three (or more) of the following six symptoms (with at least some symptoms present for more days than not for the past six months):
1. Restlessness or feeling keyed up or on edge
2. Being easily fatigued
3. Difficulty concentrating or mind going blank
4. Irritability
5. Muscle tension
6. Sleep disturbance
The anxiety causes significant distress or impairment and is not attributable to another condition or substance.
SPECIFIC PHOBIA
Specific Phobia is characterized by an intense, irrational fear of a specific object, situation, or activity that is actively avoided or endured with intense anxiety. The fear is disproportionate to the actual danger posed.
DSM-5 Criteria:
Marked fear or anxiety about a specific object or situation (e.g., flying, heights, animals, receiving an injection).
The phobic object or situation almost always provokes immediate fear or anxiety.
he object or situation is actively avoided or endured with intense fear.
The fear or anxiety is out of proportion to the actual danger posed and the sociocultural context.
The fear, anxiety, or avoidance is persistent, typically lasting for six months or more.
The condition causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
The disturbance is not better explained by another mental disorder (e.g., social anxiety disorder, OCD, PTSD).

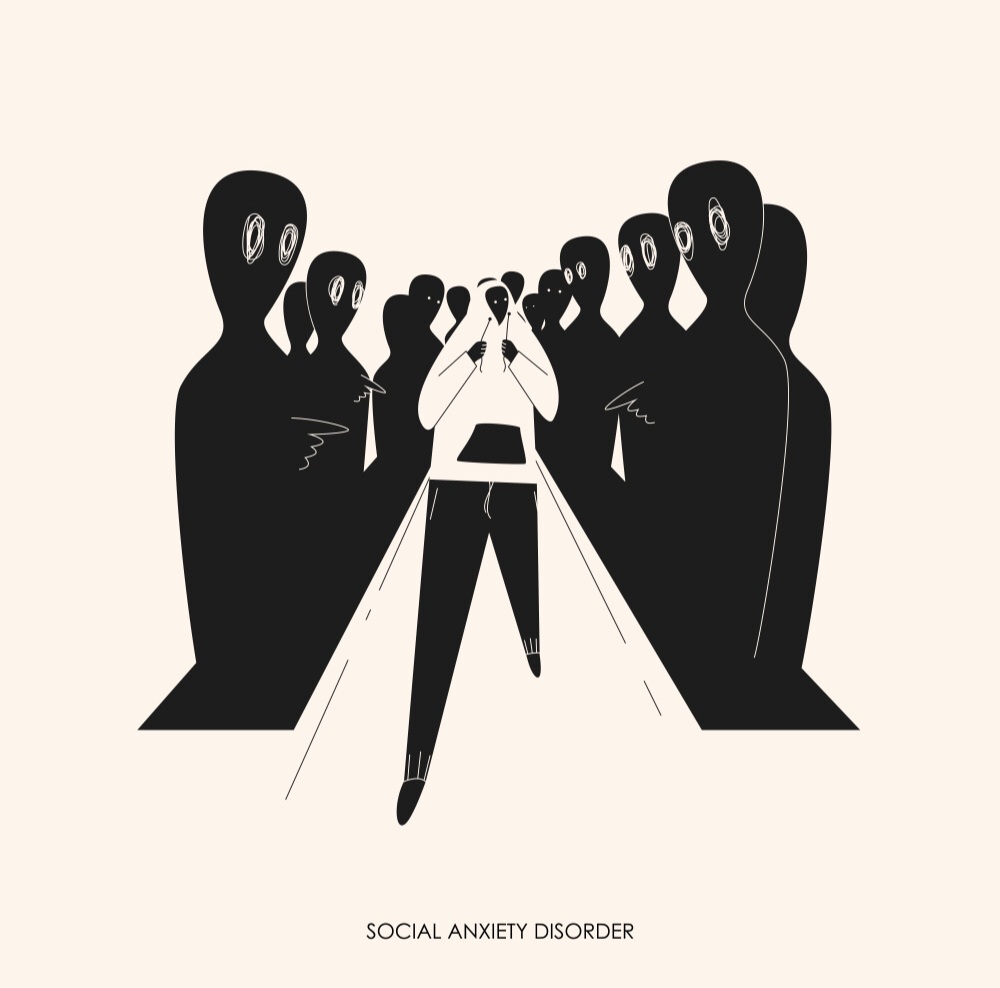
SOCIAL-ANXIETY DISORDER
Social Anxiety Disorder is characterized by intense fear or anxiety about one or more social situations in which the individual is exposed to possible scrutiny by others.
DSM-5 Criteria:
1.The individual fears that they will act in a way or show anxiety symptoms that will be negatively evaluated.
2.The social situations almost always provoke fear or anxiety and are avoided or endured with intense fear.
3.The fear or anxiety is out of proportion to the actual threat.
4.The fear, anxiety, or avoidance is persistent, typically lasting for six months or more.
The condition causes clinically significant distress or impairment and is not attributable to another medical or mental disorder.
OBSESSIVE-COMPULSIVE DISORDER
OCD is characterized by the presence of obsessions, compulsions, or both, which are time-consuming and cause significant distress or impairment.
DSM-5 Criteria:
Obsessions are defined by:
1. Recurrent and persistent thoughts, urges, or images that are intrusive and unwanted
2. The individual attempts to ignore, suppress, or neutralize them with another thought or action
Compulsions are defined by:
1. Repetitive behaviors or mental acts that the individual feels driven to perform in response to an obsession
2. The behaviors or mental acts are aimed at reducing anxiety or preventing a feared event, but are not connected in a realistic way or are clearly excessive
The obsessions or compulsions are time-consuming (e.g., more than one hour per day) or cause clinically significant distress or impairment.


POST-TRAUMATIC STRESS DISORDER
PTSD is a trauma-related disorder that can develop after exposure to actual or threatened death, serious injury, or sexual violence.
DSM-5 Criteria:
1.Exposure to trauma through direct experience, witnessing it, learning it occurred to a close person, or repeated exposure to aversive details.
2.Presence of one or more intrusive symptoms (e.g., flashbacks, distressing memories, nightmares).
3.Persistent avoidance of stimuli associated with the tratrauma
4.Negative alterations in mood and cognition (e.g., guilt, detachment, memory problems).
5.Marked alterations in arousal and reactivity (e.g., irritability, hypervigilance).
Duration of the disturbance is more than one month.
Causes significant distress or impairment and is not due to substance use or a medical condition.
DISORDER RELATED TO SOMATIC SYMPTOMS
Somatic Symptom Disorder is characterized by the presence of one or more somatic (bodily) symptoms that are distressing or result in significant disruption of daily life, along with excessive thoughts, feelings, or behaviors related to the symptoms.
DSM-5 Criteria:
One or more somatic symptoms that are distressing or significantly disrupt daily life.
Excessive thoughts, feelings, or behaviors related to the somatic symptoms, as shown by one or more of the following:
1. Disproportionate and persistent thoughts about the seriousness of symptoms
2. Persistently high level of anxiety about health or symptoms
3. Excessive time and energy devoted to these symptoms or health concerns
Although the symptom may not be continuously present, the state of being symptomatic is persistent (typically more than six months).
The disorder is not better explained by another medical or mental condition.

Common Questions
What are the most prevalent psychological disorders in Bangladesh?
In Bangladesh, the most common mental disorders reflect both global trends and unique local factors such as poverty, stigma, trauma, and limited mental health services. According to national surveys and academic studies (such as those conducted by NIMH, WHO, and icddr,b), the most common mental disorders in Bangladesh include:
1. Depressive Disorders
2. Anxiety Disorders
3. Somatic Symptom Disorders
4. Substance Use Disorders
5. Obsessive-Compulsive Disorder (OCD)
6. Post-Traumatic Stress Disorder (PTSD)
7. Schizophrenia and Other Psychotic Disorders
8. Bipolar Disorder
What are the key causes of mental disorders in Bangladesh?
Most common factors for mental disorders in Bangladesh:
1. Poverty and financial stress
2. Unemployment and job insecurity
3. Domestic violence and family conflict
4. Trauma from natural disasters or violence
5. Substance abuse
6. Lack of mental health awareness
7. Stigma around mental illness
8. Limited access to mental health services
9. Chronic physical illness1
0. Academic and social pressure (especially among youth)
What are the common techniques of treatment?
Most common factors for mental disorders in Bangladesh:
1. Poverty and financial stress
2. Unemployment and job insecurity
3. Domestic violence and family conflict
4. Trauma from natural disasters or violence
5. Substance abuse
6. Lack of mental health awareness
7. Stigma around mental illness
8. Limited access to mental health services
9. Chronic physical illness
10. Academic and social pressure (especially among youth)
The role of psychologists in treating mental disorders?
The key roles of psychologists in treating mental disorders are:
1. Assessing and diagnosing mental health conditions
2. Providing psychotherapy (individual, group, or family)
3. Developing treatment plans tailored to the client’s needs
4. Using evidence-based therapeutic techniques (e.g., CBT, DBT)
5. Monitoring client progress and adjusting interventions
6. Teaching coping strategies and problem-solving skills
7. Offering psychoeducation to clients and families
8. Supporting crisis intervention and suicide prevention
9. Collaborating with psychiatrists and other health professionals
10. Promoting mental health awareness and prevention in communities
Why choose Psychology for Today for getting help?
1.Experienced experts committed to your mental health.
2.A supportive and safe environment.
3.Personalized care based on proven methods.

